PEI Blog
How Building Decarbonization Can Transform HVAC
On 25, Mar 2022 | No Comments | In PEI Blog | By Jorlyn
ASHRAE Journal, vol. 63, no. 9, September 2021
Buildings in the US account for 40% of carbon emissions. Eighty percent of that is from electricity use and the remainder is from the combustion of fossil fuels for heating and other uses at the building. As many states, utilities, and large corporations are moving to get electricity from clean, carbon neutral sources, it is clear that electricity is becoming the carbon free choice of energy for many in the US. Buildings that use natural gas and other fossil fuels for heating will be stuck producing carbon emissions, as electricity becomes increasingly carbon free. Natural gas can now be replaced with electric systems that provide equivalent or better service. An all electric building coupled with a renewable or carbon free source of electricity is considered to be a decarbonized building.
VIEW THE FULL ARTICLE HERE
Can We Build Zero Emission Buildings?
On 11, Jan 2021 | In PEI Blog | By Peter

Variable refrigerant flow heat pumps of an all-electric HVAC system
Story at a glance:
- By the end of 2019 11 states and 160 cities had official goals to get 100% of their electricity from clean sources by 2050.
- Current typical HVAC systems can be replaced with alternative systems that use heat pumps for heating instead of gas.
- An Exelixis building in California shows the decarbonization potential.
What is building decarbonization?
Buildings in the US account for 40% of carbon emissions. And 80% of that is from electricity use; the remainder is from the combustion of fossil fuels for heating and other uses at the building.
As many states, utilities, and large corporations are moving to get electricity from clean, carbon neutral sources, it’s clear that electricity is becoming the carbon-free choice of energy for many in the US.
Buildings that use natural gas and other fossil fuels for heating will be stuck producing carbon emissions, as electricity becomes increasingly carbon-free. Natural gas can now be replaced with electric systems that provide equivalent or better service. An all-electric building coupled with a renewable or carbon-free source of electricity is considered to be a decarbonized building.
CONTINUE READING THE ARTICLE HERE
COVID-19 and Office Building HVAC Responses
On 06, Apr 2020 | In PEI Blog | By Peter
Summary of source information prepared by Point Energy Innovations
Peter Rumsey, ASHRAE Fellow, Rami Moussa, PE & Jorlyn Le Garrec
Version 7/08/20
If you would like to discuss HVAC strategies further please contact Rami Moussa at rami@pointenergyinnovations.com
Purpose
As we face these unprecedented times, it is important to address our safety and the safety of those around us without causing undue panic. As building owners, developers, engineers and architects, we have responsibility for the health and comfort of our building occupants. This document is a summary of the statements and guidance from sources in the reference and resource section as they pertain to HVAC. It is intended to be a resource to understand OFFICE Building HVAC measures and their limitations in mitigating the spread of COVID-19 (also called SARS-CoV-2) in office buildings. In this paper we summarize several simple to implement recommendations that will significantly improve the safety of buildings.
When we eventually reach the period beyond COVID-19, we have the opportunity to redefine health in buildings. Many of the changes that we make now could have lasting improvements on air quality. Improved filtration and increased outside air are but two examples of this. Building occupants and tenants will fully understand that improved health in buildings is a priority and can be one of the most valuable elements in the selection of where to work and live.
Recent Developments (as of July 1, 2020)
In an open letter to the World Health Organization (WHO) on July 6th 2020, 239 scientists from 32 countries demonstrate “beyond any reasonable doubt that viruses are released during exhalation, talking, and coughing in microdroplets small enough to remain aloft in air and pose a risk of exposure at distances beyond 1 to 2 m from an infected individual”(1).
Transmission of COVID-19
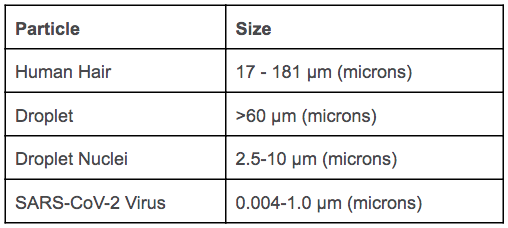
There are several modes of transmission that must be considered when looking to reduce virus transmission. Direct transmission involves direct body contact or physical transfer of infected droplets from an infected person. Indirect transmission involves contact between a person and a contaminated surface. The droplets involved in direct and indirect transmission are classified as large droplets (>60 μm) which fall about 1 m (3 ft) from infected individuals and are generally unaffected by HVAC equipment. Another form of transmission is airborne transmission, which involves a second classification of smaller droplets. These small droplets, usually 0.3 – 10 μm, are small liquid particles that are expelled during coughing, sneezing, and even talking. Through rapid desiccation (drying and breaking apart), small droplets are formed from larger droplets and become suspended in air. When these suspended droplets carry virus particles, they are called droplet nuclei.
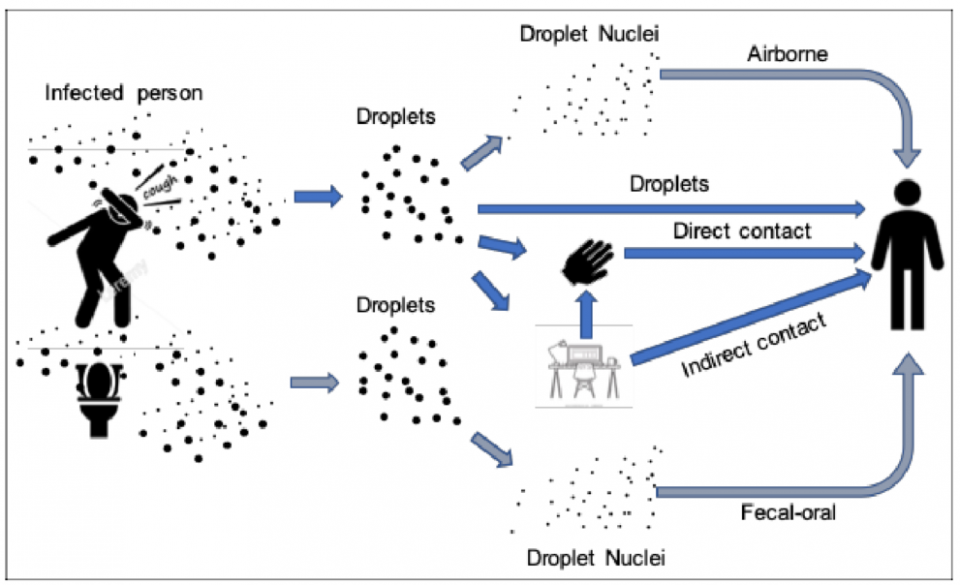
The relative importance of each transmission pathway (direct contact, indirect contract, and airborne) are still unclear and the necessary research will likely take months to confirm. In the interest of keeping buildings safe, airborne transmission should be considered important and HVAC measures should be carefully considered. However, these HVAC measures should only be one part of a comprehensive plan to reduce transmission in buildings. Other important measures to reduce transmission in office buildings are to maintain social distancing of at least 2m (6 ft) between individuals, wear cloth face coverings, regularly wash hands, disinfect potentially contaminated surfaces, and require sick individuals to stay home.
How HVAC can help prevent the spread of COVID-19
A virally infected droplet nuclei from one space can travel through ducted air pathways, leaky air filters, fans, dampers and grills, and end up in other parts of a building. The principal role of HVAC in disease transmission prevention is to remove contaminated airborne nuclei droplets from spaces and reduce the risk of spread to other spaces. ASHRAE advises that this can be accomplished through(12):
- Supplying clean air to susceptible occupants
- Containing contaminated air and/or exhausting it to the outdoors
- Diluting the air in a space with cleaner air from outdoors and/or by filtering the air
- Cleaning the air within the room
The most important guidance is preventing people who have COVID-19 from being in the building in the first place. Particle nuclei can be present in the air long before they get to filters or are exhausted out of the building.
HVAC measures to reduce transmission:
A virus particle is only dangerous if it can successfully infect a person. The primary goal in HVAC for disease prevention is to reduce occupant infection rates.The following aspects that have have an impact on infection rates are:
- Dose (the amount of virus that a person comes into contact with)
- Time (the amount of time a person is in contact with the virus)
- Virulence (virus’ ability to infect a host)
- Occupant health
Outdoor Air Ventilation
Outdoor air is a driving factor on how contaminated particles move through a space, how quickly they move, and if they move between spaces. Outdoor air is important for reducing both the time a person is in contact with the virus and the dose the person is in contact with. The figure below shows the infection rate of airborne infectious diseases based on the outdoor air (ACH or air changes per hour) and the “quantum of infection” (q or qph). Note that the “quantum of infection” is not an actual physical unit, it is a hypothetical infectious dose unit calculated from epidemiological studies. Studies show that the “q” for SARS-CoV-2 is between 14 and 48(13).
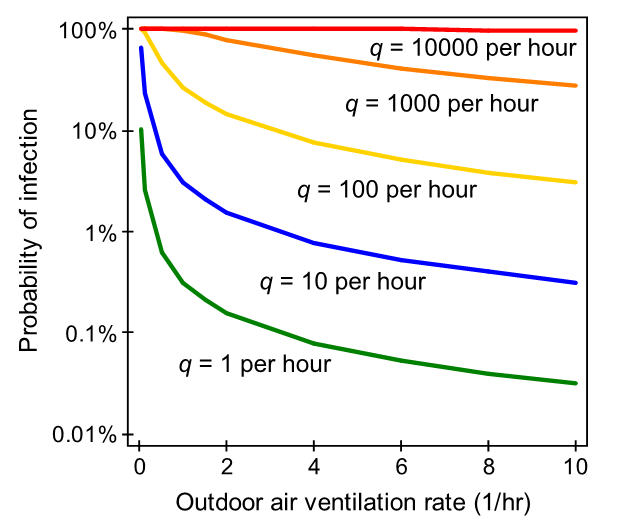
Code required outside air ventilation is around 1 ACH, which does provide reduction in probability of infection. However, based on the scientific studies and recommendations from CDC and ASHRAE, more outside air ventilation provides increased safety. In air handlers where return air is mixed with outside air, the assumption is that the return air could contain aerosolized virus particles and is not safe. Increasing the outdoor air percentage in the air handler will reduce or eliminate contaminated particles moving between spaces. More potentially contaminated air is removed from the space and replaced with uncontaminated air. Similarly, providing natural ventilation through operable windows will provide additional uncontaminated air to the space. Recirculating systems, on the other hand, will be replacing air with possibly infected air from other spaces and is not considered ventilation in and of itself.
Filtration
The goal with filtration is to reduce the dose that each occupant is exposed to. Minimum Efficiency Reporting Value (MERV) is a system used to evaluate the efficiency of an air filter based on how effective it is at catching particles of varying sizes. While SARS-CoV-2 virus particles are very small, the virus is typically only airborne when attached to a droplet nuclei (0.3-10 μm). When selecting filter efficiency, there is a tradeoff between capture efficiency and pressure drop across the filter. Research has shown that MERV 13 to 16 is the best balance for reducing infectious disease risk and reasonable operational costs(15).
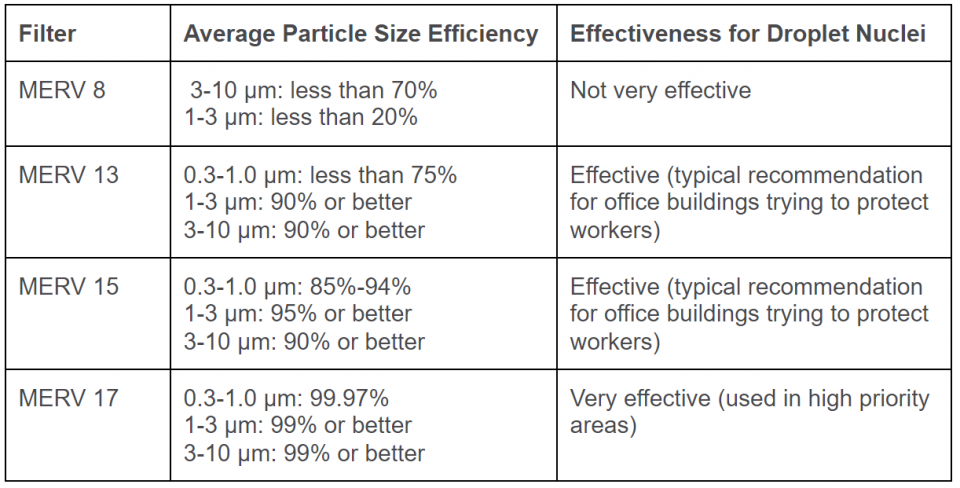
When it comes to filters, it is important to understand where the viral load is coming from relative to filter location. In office buildings the viral load comes from inside the buildings. While filters on 100% outdoor air systems are important for maintaining occupant health by filtering outdoor air pollutants and allergens, they will not reduce virus particles that originate from building occupants. However, typical mixed air ventilation systems do transfer air from one space to another when they mix return air and outside air and recirculate to the building. To reduce disease transmission in these systems, focus on increasing the capture efficiency of filters on all recirculation systems including central air handlers as well as local fan coil units.
Ultraviolet (UV) Light
While the entire UV spectrum can kill/inactivate viruses, UV-C (200-280 nm) provides the most germicidal effect. UV-C does not penetrate deeply into human tissue, however it can penetrate the outer layers of skin and eyes. When using UV in an occupied space, shielding is necessary to prevent direct exposure to the eyes.
UV works by damaging the structure of the virus to reduce the virulence and dose of the virus present. UV dose can be calculated as,
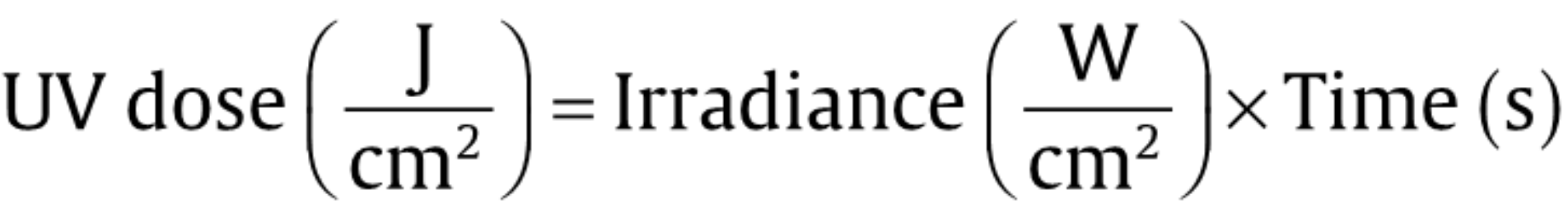
where the irradiance in the intensity of the UV light, and the time is the exposure time to the UV light. The time that UV light takes to inactivate a virus depends on many variables in the space such as exposure time, temperature, and humidity. Literature supports that exposure of 1 J/cm² is capable of decontaminating influenza virus on N95 FFRs(16). Research also shows that UV dose is even less for single strand RNA viruses (SARS-CoV-2 is a ssRNA virus) at 3-6 mJ/cm² for 99% viral reduction(17)
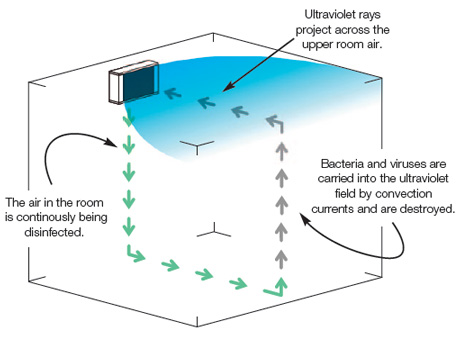
UV can be used in two different methods for disease prevention, surface ultraviolet germicidal irradiation (UVGI) and upper-room UV-C. UVGI is a method of disinfection that uses UV-C to kill viruses on surfaces such as masks, ducts, or coils. While this method does not remove airborne viruses, it can be useful to minimize growth inside the air handler or disinfect unoccupied spaces. Upper-room UV-C uses UV lights to create a disinfectant zone overhead. Airborne particles with viruses will lose virulence and ultimately be inactivated as they spend time in the disinfectant zone. This method can remove airborne contaminant load from a space without increasing outdoor air. For occupant safety, upper-room UV-C should only be used in rooms that are at least 7 feet high. While more research is needed to understand UV and SARS-CoV-2, the CDC states, “consider using ultraviolet germicidal irradiation (UVGI) as a supplement to help inactivate the virus”. ASHRAE strongly recommends upper-room UVGI (with possible in-room fans) as a supplement to airflow.
Humidity
Humidity can have an impact on the time of exposure, virulence, and occupant health. Studies show increased infection rates at low relative humidity (RH). RH below 40% can:
- Shrink infected aerosols causing them to stay airborne longer
- Increase viability of anhydrous viruses/bacteria
- Harm occupant health – impairs mucus membrane barriers
While not specific to airborne viruses, it is a general requirement to maintain an upper limit RH for building health. RH above 60% can:
- Cause microbial growth in duct systems and water reservoirs
- Cause condensation and mold growth in cold climates
Recommendations for Existing Buildings
- Filtration – Upgrade filters to a minimum of MERV 13, preferably MERV-15, filters. This will reduce the spread of virus attached to droplet nuclei in buildings where air is recirculated. MERV 13 filters are classified to capture 90% of particles of 1 μm and larger.
- All buildings with air handlers – Increase the fraction or amount of outside air as much as possible. It is important not to go above limits of what the building HVAC can handle to maintain proper humidity.
- Buildings with all air heating and cooling systems – For buildings that are capable of outside air economization (most office buildings built after the 1970s) run in 100% airside economizer mode to supply fresh air to the building and reduce or eliminate recirculated air. On extreme hot or cold days, the economizer might need to be moderated in order to maintain comfortable temperatures in the building. If so, follow the filter recommendations above.
- Buildings with operable windows – Encourage occupants to open the windows while in the building or set controls to open motorized windows during occupied hours. This might not be possible or desirable on cold winter days or hot and humid days. This will allow for the maximum amount of outside air to flush the building.
- Buildings with recirculating fan coils such as VRF systems – Change filters on the fan coils to a minimum of MERV 13, preferably MERV 15. This might reduce the heating and cooling capacity of the fan coils on the peak days.
- Buildings with Demand Control Ventilation (DCV) – Disable DCV and allow for the maximum amount of outside air in spaces that have high occupancy. In other spaces, such as spaces with low occupancy due to social distancing, increase the DCV setpoints.
- Toilet Rooms – Keep toilet exhaust on 24/7 to reduce risk of fecal-oral transmission. Ultraviolet recommendation below.
- Humidifiers – If humidifiers are already present in an HVAC system, humidify the building to above 40%. This has been shown to reduce the formation of droplet nuclei. Humidification is normally only needed when temperatures outside are colder. It is possible but difficult to add humidifiers to ducts or air handlers if they aren’t already present.
- Ultraviolet germicidal irradiation (UVGI) – Add upper-room UV-C in high density spaces such as lobbies, conference rooms, and restrooms. UV-C takes time to inactivate contaminants in air so it will be most beneficial in high density spaces where people spend extended periods of time. Also consider upper-room UV-C in spaces that are unable or impractical to increase outdoor air. With good filtration, as recommended above, in duct or air handler UVGI is not necessary.
- Elevators – Limit the number of people allowed in each elevator and designate locations for each person to stand. Most elevators do have exhaust fans that exhaust into the liftway (or elevator shaft). The liftway should be kept under negative pressure with the liftway exhaust fan (required in most newer buildings). Both of these fan systems should be serviced and verified for proper operation.
Where exhaust fans don’t exist, add localized UV-C lighting and/or small filter systems to elevator cabs. - Maintenance – Building operators should be aware of possible duct and filter contamination. Maintenance technicians should adhere to recognized standards and procedures and wear PPE (Personal Protective Equipment) and P2 mask with respirator when servicing and changing filters. If safe for staff, all normal preventative maintenance should continue in order to ensure proper operation of HVAC systems.
- Controls – If the building controls are not maintained and operating correctly, other measures taken may have no effect. Test and recommission all ventilation, temperature and humidity controls to ensure proper operation of the ventilation system and air side economizer system.
- Energy – Generally, many of the recommendations will result in higher energy use. While unfortunate, we see these recommendations as temporary. Once the virus has passed, returning parts of the system back to normal operation will be possible and recommended. For buildings that have been shut down due to transmission concerns, HVAC equipment serving non critical spaces can be turned off or turned down to save energy. Of course, in some climates, maintaining temperatures in the building that prevent freezing or overheating might require that equipment is left on, but temperature setpoints are adjusted.
Recommendations for New Construction Office Buildings
In addition to the ideas listed for existing buildings, when looking at new construction the following should be considered:
System Selection
- Economizer – Favor systems that are capable of providing 100% economizer operation. VAV systems are a good example of this.
- Dedicated Ventilation – Consider systems that use dedicated outside air (DOAS) and do not recirculate air. DOAS systems can be sized for additional air flow during pandemics. Aerosolized particles do not get recirculated through other parts of the building. A low cost option would be to upsize a DOAS by 50% to 100%. DOAS systems are typically coupled with other systems that provide heating and cooling such as VRF fan coils or radiant panels.
- Displacement Systems – Consider systems that supply air conditioning air or ventilation air from the low points in the occupied space will avoid the mixing in the thermal zone where aerosolized particles can move through a room. Raised floor systems or sidewall displacement systems are well developed and have documented health, comfort and indoor air quality advantages beyond virus protection.
Other Measures
- Air pathways – Plan air pathways through the building. Minimize air turbulence and air that passes direct from person to person. Strategic use of return diffusers and return ductwork can lower exposure between zones.
- Ultraviolet germicidal irradiation (UVGI) – Add upper-room UV-C in high density spaces such as lobbies, conference rooms, and restrooms. UV-C takes time to inactivate contaminants in air so it will be most beneficial in high density spaces where people spend extended periods of time. Also consider upper-room UV-C in spaces that are unable or impractical to increase outdoor air. With good filtration, as recommended above, in duct or air handler UVGI is not necessary. When designed into new buildings, these systems can be hidden from occupant view and only used during periods of concern.
- Humidifiers – Provide humidity control strategies to maintain building relative humidity (RH) above 40% (note that it is not recommended to exceed 60% RH due to other health concerns such as mold growth).
- Controls – Fully commission the HVAC control systems on all projects. Special attention should be paid to systems such as economizers that are essential to bringing in outside air.
Disclaimer
Point Energy Innovations is providing this information as a service to the general community. We are not infectious disease transmission experts. All strategies and statements in this document should be verified by each individual or organization using their own sources of information. This document is a summary of statements and guidance from sources listed in the references and resource section. These recommendations are focused on office buildings only. We recommend that an Environmental Health and Safety expert be consulted before taking action. Reliance on any information provided herein is solely at your own risk. Best practices on HVAC systems should in no way be substituted for social distancing or any other recommendations from the NIH and CDC. HVAC system improvements will not reduce surface related transmission, and therefore cannot on their own make a building safe. This Resource Paper is highly general and introductory in nature and is not intended nor authorized for any project-specific use. This paper may also contain unintended errors. Point Energy Innovations disclaims liability for any use of this Resource Paper that is not explicitly authorized in writing by Point Energy Innovations.
If you would like to discuss HVAC strategies further please contact Rami Moussa at rami@pointenergyinnovations.com
References and Resources
- Morawska, Lidia, Milton, Donald K. It is Time to Address Airborne Transmission of COVID-19, https://academic.oup.com/cid/article/doi/10.1093/cid/ciaa939/5867798.
- Federation of European Heating, Ventilation and Air Conditioning Associations (REHVA). REHVA COVID-19 Guidance Document. March 17, 2020, www.rehva.eu/activities/covid-19-guidance.
- Coronavirus. World Health Organization (WHO). https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
- Lu, J. et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. https://doi.org/10.3201/eid2607.200764.
- Hamner L, Dubbel P, Capron I, et al. High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice – Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:606–610. http://dx.doi.org/10.15585/mmwr.mm6919e6
- Santarpia, J. L., Rivera, D. N., Herrera, V., Morwitzer, M. J., Creager, H., Santarpia, G. W., … Lawler, J. V. (2020). Transmission potential of SARS‐CoV‐2 in viral shedding observed at the university of Nebraska medical center. medRxiv . Preprint. https://doi.org/10.1101/2020.03.23.20039446
- Liu, Y., Ning, Z., Chen, Y. et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 582, 557–560 (2020). https://doi.org/10.1038/s41586-020-2271-3
-
Patrick F Horve, Leslie Dietz, et al. Identification of SARS-CoV-2 RNA in Healthcare Heating, Ventilation, and Air Conditioning Units. https://doi.org/10.1101/2020.06.26.20141085
-
Teunis PF, Brienen N, Kretzschmar ME. High infectivity and pathogenicity of influenza A virus via aerosol and droplet transmission, Epidemics, 2010, vol. 2 (pg. 215-22)
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook MG, Gamble A., Williamson B.N., et al. Aerosol and Surface Stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine, March 17, 2020, www.nejm.org/doi/full/10.1056/NEJMc2004973.
- Morawska, J. Cao. June 2020. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int., 139 (2020), Article 105730. https://www.sciencedirect.com/science/article/pii/S016041202031254X
-
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE). The ASHRAE Position Document on Infectious Aerosols. Approved by ASHRAE Board of Directors, April 14, 2020, www.ashrae.org.
- Hui Dai, Bin Zhao. Associated of infected probability of COVID-19 with ventilation rates in confined spaces: a Wells-Riley equation based investigation.
-
Stephens, B. (2012). HVAC filtration and the Wells-Riley approach to assessing risks of infectious airborne diseases. National filtration Association (NAFA) Foundation Report.
-
P. Asimi, B. Stephens, HVAC filtration for controlling infectious airborne disease transmission in indoor environments: predicting risk reductions and operational costs, Build. Environ. 10 (2013) 150-160, https://doi.org/10.1016/j.buildenv.2013.08.025
- Lindsley, W. G., Martin, S. B., Thewlis, R. E., Sarkisian, K., Nwoko, J. O., Mead, K. R., et al. (2015). Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. Journal of Occupational and Environmental Hygiene, 12(8), 509–517. https://www.tandfonline.com/doi/abs/10.1080/15459624.2015.1018518.
- Tseng, C. C., & Li, C. S. (2007). Inactivation of viruses on surfaces by Ultraviolet Germicidal Irradiation. Journal of Occupational and Environmental Hygiene, 4, 400-405
- Dietz, L., Horve, P.F., Coil, D., Fretz, M., Eisen, J., Van Den Wymelenberg, K. 2019 Novel Coronavirus (COVID-19) Outbreak: A Review of the Current Literature and Built Environment (BE) Considerations to Reduce Transmission. March 20, 2020, www.preprints.org/manuscript/202003.0197/v2.
- Dixon, Keenan. Air Filtration and COVID-19: Indoor Air Quality Expert Explains How to Keep You and Your Building Safe. The University of Toronto Engineering News, March 20, 2020, news.engineering.utoronto.ca/air-filtration-and-covid-19-indoor-air-quality-expert-explains-how-to-keep-you-and-your-building-safe.
- Center for Disease Control & Prevention (CDC). Summary List for Healthcare Facilities: Strategies for Optimizing the Supply of N95 Respirators during the COVID-19 Response. March 5, 2020, www.cdc.gov/coronavirus/2019-ncov/hcp/checklist-n95-strategy.html.
- The National Institutes of Health (NIH). New Coronavirus Stable for Hours on Surfaces. March 17, 2020, www.nih.gov/news-events/news-releases/new-coronavirus-stable-hours-surfaces.
- A.G. Coombs. HVAC and COVID-19. March 18, 2020, https://www.agcoombs.com.au/news-and-publications/advisory-notes/hvac-and-covid-19.
- The American Institute of Architects (AIA). May 28,2020. Re-Occupancy Assessment Tool V2.0. https://www.aia.org/resources/6292441-re-occupancy-assessment-tool
- Center for Disease Control & Prevention (CDC). COVID-19 Employer Information for Office Buildings. https://www.cdc.gov/coronavirus/2019-ncov/community/office-buildings.html

